
While food allergy testing at home can feel like a convenient first step in figuring out your symptoms, it's really important to know what these kits can and can't do. They are not a definitive diagnosis for a true food allergy. Think of them as a tool to gather some preliminary clues, opening the door for a more productive conversation with your doctor—not as the final word on what you can or can't eat.
Should You Try Food Allergy Testing at Home?

If you've ever felt bloated after dinner, dealt with a surprise rash, or just felt off after eating certain foods, the thought "Could this be a food allergy?" has probably crossed your mind. That question often leads people straight to the world of at-home food allergy tests, which have become a popular and easy-to-find option.
This isn't just a niche trend; the market is booming. A global rise in allergies and our collective desire for accessible health answers are fueling major growth. In fact, projections show the at-home allergy test kit market could hit around USD 2.5 billion by the end of 2025, largely driven by how simple it is to buy them online. You can see more data on the at-home test kit market growth on datainsightsmarket.com.
But before you click "add to cart," it's crucial to manage your expectations.
Understanding What These Tests Actually Measure
Here's the most important thing to understand: most at-home tests are looking for something completely different than what a board-certified allergist tests for.
Let's break down that distinction, because it’s everything.
- A True Food Allergy (IgE-Mediated): This is a serious immune system response. Your body wrongly flags a food protein as a major threat and unleashes Immunoglobulin E (IgE) antibodies to attack it. This triggers an immediate, and sometimes life-threatening, reaction like hives, swelling, difficulty breathing, or even anaphylaxis.
- A Food Sensitivity (Often Measured by IgG): This is what many at-home kits test for—Immunoglobulin G (IgG) antibodies. Unlike the IgE "attack" antibodies, the presence of IgG often just means your body has been exposed to a food. It's a sign of memory, not necessarily a sign of a problem causing your symptoms.
Think of it this way: An IgE reaction is like a blaring fire alarm signaling immediate, clear danger. An IgG result is more like seeing a familiar face in a crowd—it just shows recognition, not that anything is wrong.
The Real Role of an At-Home Test
So, where does that leave you? An at-home food allergy test can still be a useful tool, as long as you use it correctly. It’s a starting point for gathering data. The results might point to a few foods that you can then track more carefully with a food and symptom journal.
This information empowers you to walk into your doctor's office with more than just a vague feeling of "I don't feel well." You can show them the test results alongside your own observations, creating a much clearer picture. This focused approach helps your doctor decide on the right next steps, like ordering clinical testing, potentially saving you a lot of time and frustration on your path to feeling better.
How At Home Allergy Tests Actually Work

So, you’ve decided to take matters into your own hands and try an at-home test. But what really goes on between that tiny finger prick and the detailed report that lands in your inbox? It's a surprisingly simple process that turns your kitchen table into the first step of a personal scientific investigation.
It all starts when you order a kit, like the popular BARB N.P. Food Allergy Test, which arrives with everything you need. The most important step is collecting a small blood sample. Don't worry, it's not as intimidating as it sounds. The kit includes a sterile lancet for a quick, tiny prick on your fingertip—just enough to collect a few drops of blood on a special collection card.
Once your sample is collected and dried, you'll pop it into the pre-paid mailer and send it off to a CLIA-certified laboratory. This certification is a big deal; it means the lab adheres to high federal standards for quality and accuracy. At the lab, technicians get to work, analyzing how your blood sample interacts with a whole host of different food proteins. For a closer look at what to expect, check out our full guide to allergy testing at home.
The Lock and Key Science
To really get what the lab is looking for, it helps to think of your immune system like a "lock and key" system. Every food protein is a unique "lock," and your body creates specific antibodies that act as the "keys."
But here's the crucial part: not all keys do the same thing.
-
IgE Antibodies (The Allergy Key): These are the keys tied to a true food allergy. When an IgE antibody clicks into a food protein lock, it triggers an immediate and sometimes severe reaction—think hives, swelling, or worse. This is your body's five-alarm fire bell.
-
IgG Antibodies (The Exposure Key): These are the keys that most at-home "sensitivity" tests measure. When an IgG antibody fits a food protein lock, it's usually just a sign that you’ve been exposed to that food. It’s more like a memory marker than an actual alarm.
The presence of IgG doesn't automatically mean a food is the culprit behind your symptoms. In fact, high IgG levels can simply mean you eat that food often and your body has a perfectly normal, healthy tolerance for it.
Your test report is a snapshot of these antibody interactions. It shows which "keys" (antibodies) were found in your blood and how strongly they reacted to the different "locks" (food proteins).
This distinction is the single most important thing to grasp when you get your results. A test showing high IgG reactivity to wheat doesn't mean you have a wheat allergy; it just notes that your immune system remembers seeing wheat before. Understanding this foundation is what empowers you to read your report with a critical eye and have a much more productive conversation with your doctor.
Comparing IgE and IgG At Home Tests
When you start digging into at-home food allergy tests, you’ll quickly run into two acronyms: IgE and IgG. These aren't just technical jargon; they represent completely different ways your body can respond to food. Getting this distinction right is the single most important step in picking a useful test and understanding what its results actually mean.
Think of it like choosing the right tool for a job. If you have a leaky pipe, you need a wrench, not a hammer. In the same way, if you suspect a true, immediate allergy, an IgE test is the right tool. An IgG test? That's designed for something entirely different.
This image helps break down some of the key differences you’ll find between at-home tests and traditional lab-based testing.
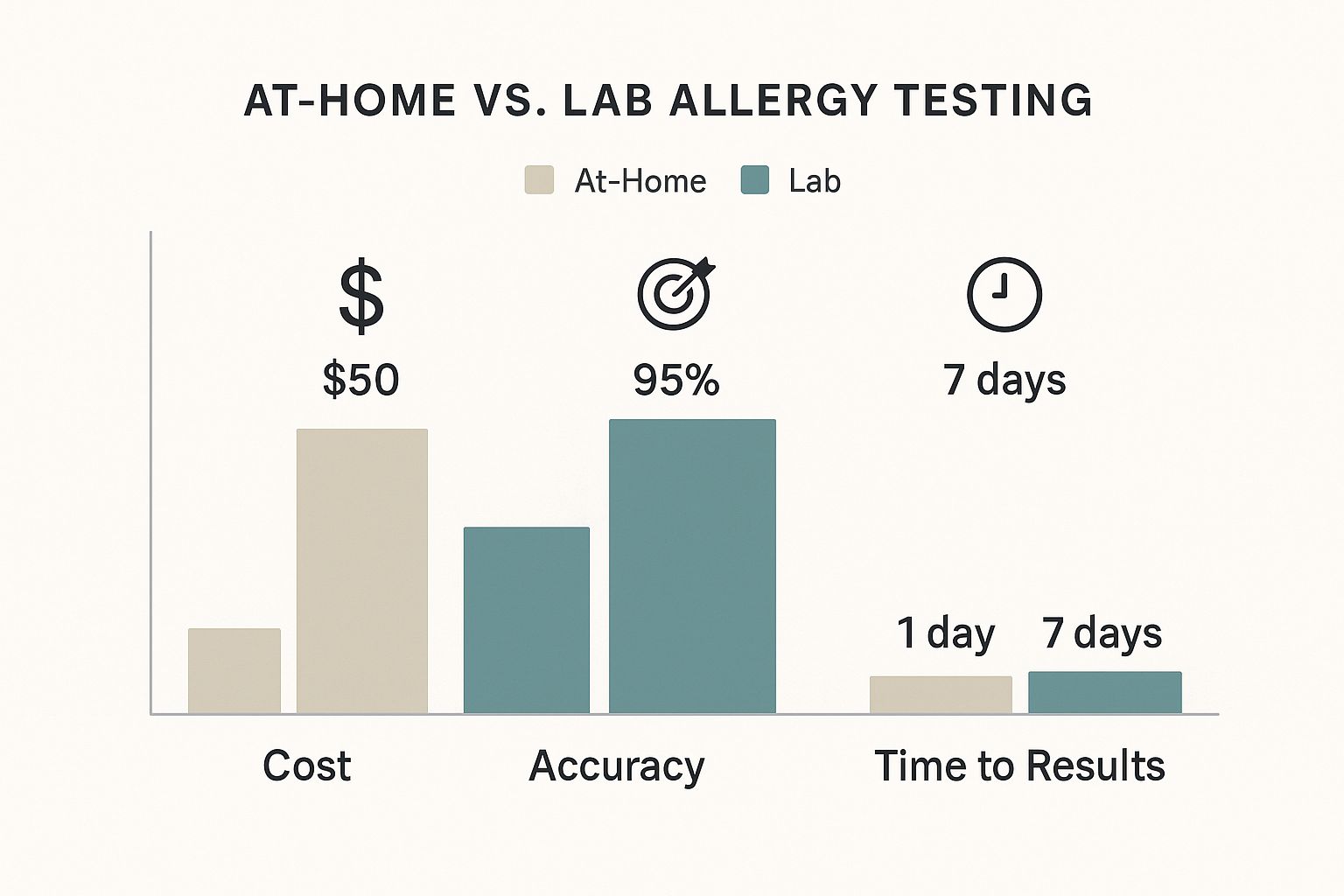
As you can see, while at-home options get you faster results and often cost less, this convenience can come at the expense of the accuracy you’d get from professional lab testing.
The IgE Test: The True Allergy Indicator
Immunoglobulin E (IgE) antibodies are your immune system’s first responders—the emergency alarm. When you have a true food allergy, your body wrongly flags a harmless food protein as a dangerous threat. In response, it creates specific IgE antibodies that latch onto your immune cells, ready for a fight.
The next time you eat that food, the protein locks onto these IgE antibodies, triggering a rapid release of chemicals like histamine. This is what causes an immediate and sometimes severe allergic reaction.
Symptoms of a true IgE-mediated allergy include:
- Hives, intense itching, or eczema flare-ups
- Swelling of the lips, face, or throat
- Wheezing, coughing, or trouble breathing
- Anaphylaxis, a life-threatening, full-body reaction
At-home IgE tests are designed to spot these specific antibodies in your blood. A positive result doesn't give you a final diagnosis, but it does signal a potential allergic reaction—a critical piece of data to bring to an allergist.
The IgG Test: The Controversial "Sensitivity" Marker
On the flip side, most at-home tests marketed for "food sensitivity" measure Immunoglobulin G (IgG) antibodies. IgG is the most common antibody in your blood, and its main job is to create an immune "memory" of things you've been exposed to. So, high levels of IgG to a food like wheat or dairy often just mean you eat it a lot.
Unlike the clear alarm signal of an IgE reaction, the medical community widely agrees that the presence of IgG antibodies does not reliably point to a food sensitivity or intolerance. It's more like a logbook of what you've eaten, not a list of problems.
This is exactly why IgG tests can be so misleading. They frequently spit out a long list of "reactive" foods that aren't actually causing you any symptoms. Following these results without a doctor's guidance can lead to overly restrictive diets that are not only unnecessary but potentially unhealthy.
With more people trying to understand their bodies, the global food allergen testing market is booming. It's expected to jump from USD 970.3 million in 2025 to over USD 2 billion by 2035. You can learn more about food allergen market trends on futuremarketinsights.com, but this growth highlights the urgent need for clarity. When choosing a test, consider options like the BARB N.P. Food Allergy Test, which focuses on scientifically validated markers.
Comparison of At-Home Test Types
To make the distinction clearer, let's break down the core differences between IgE and IgG tests in a side-by-side comparison. This will help you see exactly what each test is—and isn't—designed to do.
| Feature | IgE Antibody Tests | IgG Antibody Tests |
|---|---|---|
| What It Measures | Antibodies linked to immediate, true allergic reactions (e.g., hives, anaphylaxis). | Antibodies indicating exposure or immune memory to a food, not a true allergy or sensitivity. |
| Scientific Backing | Widely accepted and used by allergists as a tool to help diagnose true food allergies. | Not recognized by major allergy and immunology organizations for diagnosing food sensitivities. |
| Interpretation | A positive result suggests a potential allergy and warrants a follow-up with a medical professional. | A positive result often just means you've eaten that food; it doesn't correlate with symptoms. |
| Common Use Case | Investigating symptoms that appear quickly after eating, such as swelling, itching, or wheezing. | Marketed for vague, delayed symptoms like bloating or fatigue, but the connection is unproven. |
| Potential Outcome | Provides valuable data to discuss with a doctor for a definitive diagnosis and management plan. | Can lead to unnecessary food restrictions and nutritional deficiencies without medical benefit. |
Ultimately, choosing the right test comes down to understanding the science. IgE tests offer a starting point for investigating true allergies, while IgG tests measure something else entirely—exposure—which can easily be misinterpreted as a problem.
The Truth About At Home Test Accuracy

This is the big question, isn't it? Can you actually trust the results you get from an at-home test? The answer is a little more complicated than a simple yes or no. The technology used in certified labs is excellent at what it’s designed to do—accurately detect the presence and quantity of certain antibodies in your blood.
The real challenge isn't in the detection, but in the interpretation. This is especially true for IgG tests, which are the most common type you'll find in at-home "sensitivity" kits.
Here's the problem: a positive IgG result for a food like almonds or eggs doesn't automatically mean you have a sensitivity. In many cases, it simply means you've been exposed to that food, and your immune system created a normal, healthy memory of it. It’s doing its job.
This disconnect between a "positive" result and an actual health problem is where the risk lies. The results can be a minefield of false positives.
The Problem with False Positives
A false positive is when a test flags a food as problematic, but it isn’t actually causing you any symptoms. With IgG testing, this is incredibly common.
Your lab report might come back with a long list of "reactive" foods, making you think you need to overhaul your entire diet. This can cause more harm than good.
Following a report like that without professional guidance could lead you to cut out perfectly healthy and nutritious foods for no reason. Eliminating entire food groups like dairy, grains, or certain vegetables based on a test alone can create nutritional gaps and add a huge amount of stress to your daily life. It can also cultivate an unhealthy fear around eating.
Think of a test result as a single clue in a much larger mystery. It’s one piece of data, but it's not the whole story. It cannot replace your lived experience or the expertise of a medical professional.
Viewing Your Test as a Guide, Not a Diagnosis
So, how should you approach food allergy testing at home? The healthiest mindset is to see it as a tool to start a conversation, not a final diagnosis.
The results can help you identify a few potential culprits that you can then track more carefully. For example, if your test shows high reactivity to yeast, you could start a detailed food and symptom journal to see if you actually feel worse after eating bread or drinking beer.
This approach transforms the test from a confusing list of "don'ts" into a starting point for a productive discussion with your doctor or a registered dietitian. An excellent resource for digging deeper into this is our guide on understanding food sensitivity testing accuracy, which provides more context on what your results truly mean.
Ultimately, at-home kits like the BARB N.P. Food Allergy Test are best used to gather preliminary information. They help you focus your investigation and give you specific points to bring up with a healthcare provider. They are not a substitute for a professional medical evaluation, which is essential for an accurate diagnosis and a safe, effective management plan.
What to Do with Your Test Results
The email finally lands in your inbox. Inside is your report—a digital file packed with colorful charts and a long list of foods. You’ve done the food allergy testing at home, and now you have the data. But staring at a list of "reactive" foods can feel overwhelming, maybe even a little scary.
First thing's first: take a deep breath. It's crucial not to make any sudden, drastic changes to your diet based on this report alone. Think of it less as a set of strict commands and more as a collection of interesting clues. Cutting out multiple foods all at once can lead to nutritional gaps and a whole lot of unnecessary stress around mealtimes.
Remember, a positive result—especially from an IgG test—often just means you’ve been exposed to a food, not that it's the root cause of your symptoms. The real work starts now: connecting these clues to your real-life experiences.
Turning Data into Actionable Insight
Your most powerful tool from here on out is a simple food and symptom journal. This is how you connect the dots between what the test suggests and how your body actually feels. For the next few weeks, get detailed. Log everything you eat, what time you eat it, and any symptoms that pop up.
Did your test flag dairy? Now’s the time to pay extra close attention to how you feel after that morning latte or a slice of cheese. If you start noticing a consistent pattern—say, bloating or a skin flare-up every time you have dairy—you’ve just found a meaningful correlation. That real-world evidence is worth far more than the test result on its own.
This process is a lot like a guided elimination diet, which is a highly effective way to pinpoint trigger foods. You can learn more about how to do this correctly in our comprehensive guide on using an elimination diet for food allergies.
Preparing for Your Doctor's Visit
Once you have both your test results and your food journal, you're ready for a productive conversation with an allergist or your healthcare provider. This prep work is so important. The U.S. food allergen testing market was valued at USD 315.4 million in 2025 and is only getting bigger. This growth, largely driven by immunoassay technologies that hold a 46.44% market share, means more people are getting tested, making it vital to use these results wisely. You can discover more insights about the U.S. food allergen testing market on mordorintelligence.com.
Don't just hand over the papers at your appointment. Walk in with a clear list of specific questions. This is how you turn a potentially confusing data sheet into a solid starting point for a real diagnosis.
Here are some key questions to ask your doctor:
- Based on my test results and my symptom journal, what do you think might be going on?
- Do you think these results point toward a true IgE allergy, or is it more likely an intolerance or sensitivity?
- What are the next steps for getting a definitive diagnosis? Should we consider a clinical blood test, a skin prick test, or even a medically supervised food challenge?
- For now, should I keep eating the foods that were flagged, especially if we need to do more testing?
Taking this structured approach changes everything. Your at-home test goes from being a source of anxiety to a valuable tool that helps you get the professional medical guidance you really need.
Tackling Skin Flare-Ups During Your Food Journey
It’s incredibly frustrating when your body decides to broadcast its internal struggles all over your skin. Eczema, hives, and persistent redness are often the first visible signs that something you’re eating isn't sitting right. While you’re doing the hard work of uncovering potential triggers with food allergy testing at home, you don’t have to just suffer through the uncomfortable skin symptoms.
Taking a two-pronged approach is always best. As you work with a professional on the dietary side of things, you can also give your skin the support it needs to calm down and heal. One of the simplest, non-invasive tools you can add to your routine is an at-home light therapy device like the BARB N.P. LED Facial Mask.
This mask is designed to be a soothing ally for your skin while you figure out the root cause of the irritation.
Soothe Your Skin While You Investigate
The BARB N.P. mask was created for real life—it’s completely wireless, so you can wear it while making tea or catching up on emails. It’s also lightweight and comfortable. The real magic, though, is in its three targeted light settings, each designed to tackle a different skin concern.
- Red Light: Think of this as the anti-inflammatory setting. It helps calm angry, reactive skin and supports your skin's natural healing process—perfect for those red, itchy flare-ups.
- Blue Light: If your skin issues are showing up as acne-like bumps or breakouts, the blue light helps target the specific bacteria that cause them.
- Yellow Light: This is your go-to for reducing overall redness and soothing sensitivity. It helps bring down that flushed, irritated look and feel.
Using a supportive therapy like LED treatment isn't a substitute for getting to the bottom of your dietary triggers. Instead, it complements that investigation. It’s a powerful way to manage the frustrating external symptoms while you and your healthcare provider work on solving the internal puzzle.
Your Top Questions About At-Home Food Allergy Tests, Answered
When you're trying to figure out what's causing your symptoms, diving into the world of at-home food allergy testing can feel overwhelming. You've got questions, and you need clear, straightforward answers to make the best decisions for your health. Let’s cut through the noise.
Can an At-Home Test Diagnose a Severe Food Allergy?
Let’s be crystal clear on this: No. This is the most important thing to understand. At-home kits are not designed or equipped to diagnose a true, life-threatening food allergy—the kind that can cause anaphylaxis.
If you ever experience immediate, severe symptoms like hives, swelling of the lips or tongue, or trouble breathing after eating, that’s a medical emergency. You need to see a board-certified allergist for proper clinical testing, like a skin prick test or a medically supervised oral food challenge. Don't guess.
My IgG Test Flagged a Food. Should I Stop Eating It?
Hold on a second. It's tempting to see a high IgG result and immediately banish that food from your kitchen, but it’s rarely that simple. A high IgG level for a specific food often just means you eat it regularly—it shows exposure, not necessarily a problematic sensitivity.
This is why leading medical organizations often advise against using these tests to dictate your diet. Cutting out foods based only on an IgG result can lead to unnecessary restrictions, nutritional gaps, and a lot of frustration. The smarter approach? Talk to your doctor and use a detailed food and symptom journal to connect the dots between what you eat and how you actually feel.
The difference between an allergy and a sensitivity is huge. A true food allergy is a rapid immune response driven by IgE antibodies, which can trigger those dangerous, immediate reactions. Food sensitivities or intolerances, on the other hand, are often linked to the digestive system or IgG antibodies, causing delayed and less severe symptoms like bloating, headaches, or fatigue.
Think of at-home test results as a conversation starter, not a diagnosis. They can give you clues, but they aren’t the final word. This mindset helps you get the right support without sacrificing your nutritional well-being.
For a holistic approach to your wellness journey, consider the premium health and skincare solutions offered by BotoxBarb. Explore our curated selection of medical-grade products and at-home testing options to support your goals. Learn more and shop now at https://barbnp.shop.

