
Figuring out which foods are causing you trouble takes a bit of detective work. It's a mix of careful symptom tracking, a structured elimination diet, and sometimes, a little help from modern diagnostic testing. The most important part is learning to meticulously observe your body's reactions—things like bloating, fatigue, or skin issues—and connecting what you eat with how you feel.
Decoding Your Body's Signals

Have you ever finished a meal only to feel sluggish, bloated, or mentally foggy for hours? It’s frustrating. You start wondering if it was the bread, the cheese, or something else entirely. This is the reality for so many people trying to understand their body's unique language.
The first step is to get clear on the difference between a food allergy and a food sensitivity. They feel very different and involve separate systems in your body.
- Food Allergies: These are immediate, sometimes severe, immune system responses. An allergic reaction, like hives or trouble breathing after eating peanuts, happens fast because your body flags a food protein as a major threat.
- Food Sensitivities: These are typically delayed reactions from your digestive system. Symptoms like joint pain, headaches, or skin rashes might not show up for hours—or even up to 72 hours—after you've eaten the trigger food.
This delayed onset is exactly why pinpointing a sensitivity can feel impossible. You might blame Tuesday's dinner for how you feel on Thursday, never making the real connection. If you want to dive deeper, you can explore the key differences between food intolerance and allergy in our detailed guide.
Why Are Food Sensitivities on the Rise?
It’s not just you; food-related reactions are becoming way more common. Food sensitivities and allergies now affect an estimated 220 million people worldwide. It's a huge issue, and for many, it starts in adulthood—over 50% of adults with food allergies developed them after age 18.
This trend points to a complex mix of environmental factors, modern dietary habits, and changes in our gut health. As our food supply and lifestyles evolve, our bodies can struggle to keep up, leading to low-grade inflammation and persistent discomfort.
Your Roadmap to Getting Answers
The good news is you don't have to live with the guesswork. There are proven methods you can use to gather real evidence and finally understand what your body is trying to tell you.
The goal isn't just to find out what you can't eat. It's about discovering a way of eating that makes you feel vibrant, energized, and clear-headed every single day.
There are three main strategies to choose from, each with its own benefits.
Methods for Identifying Food Sensitivities at a Glance
To help you decide on the best starting point, here’s a quick comparison of the three primary approaches to pinpointing food triggers. Each one requires a different level of commitment and offers varying degrees of accuracy.
| Method | What It Involves | Pros | Cons |
|---|---|---|---|
| Symptom Tracking | Keeping a detailed daily log of all foods eaten and any physical or mental symptoms that appear. | Low-cost and non-invasive. Helps you become more in tune with your body. | Can be time-consuming. Correlation doesn't always equal causation, especially with delayed reactions. |
| Elimination Diet | Temporarily removing common trigger foods (like gluten, dairy, soy) for a few weeks, then reintroducing them one by one. | Considered the "gold standard" for accuracy. Directly identifies cause-and-effect reactions. | Requires significant commitment, planning, and discipline. Can be socially challenging. |
| Diagnostic Testing | Using an at-home blood test (like an IgG panel) to measure your body's antibody response to a wide range of foods. | Provides data-driven insights to guide a more targeted elimination diet. Saves time by narrowing down potential culprits. | Can produce false positives and isn't a definitive diagnosis on its own. Best used as a guide, not a final answer. |
Ultimately, the best approach is often a combination. Many people start with a test to get a targeted list, then use a modified elimination diet to confirm the results. No matter which path you choose, you're taking a powerful step toward reclaiming your well-being.
Becoming Your Own Health Detective
The journey to figuring out your food sensitivities starts with one surprisingly simple tool: a food and symptom diary. You need to think of yourself as a detective, and your body is the scene of the crime. Your mission is to connect the dots between what you eat and how you feel, turning those vague feelings of "off-ness" into clues you can actually work with.
This is about more than just scribbling down "salad for lunch." To get anywhere, you need details. The goal over the next two to four weeks is to build a clear picture of your body's unique responses. This consistent, detailed tracking is the foundation for everything that comes next.
What to Track for Maximum Insight
A truly useful food diary is all about the specifics. The more detail you capture, the clearer the patterns become. Make it a habit to log these key things for every single meal, snack, and drink.
- Specific Foods and Ingredients: Don't just write "pasta." Get granular: "whole wheat spaghetti with tomato sauce, garlic, onion, and Parmesan cheese." This lets you pinpoint individual suspects.
- Portion Sizes: Did you have a small handful of almonds or half the bag? Quantity really matters. A tiny bit of a trigger food might not cause a peep, but a larger portion could be a whole different story.
- Meal Times: Note the exact time you eat. This is critical because some reactions are sneaky and don't show up for hours—or even days. Symptoms can appear up to 72 hours after you've eaten something.
- Symptoms and Timing: Write down any physical or mental shifts you notice. Get specific about when they happen in relation to your meals.
- Symptom Severity: Use a simple 1-10 scale to rate how intense your symptoms are. For example, "bloating rated 7/10 two hours after lunch."
When you gather this level of detail, you stop guessing and start building a real case file. You're no longer just pointing fingers at a food; you have the evidence to back it up.
Real-World Diary Examples
Let's see what this looks like in practice. A generic entry like "felt tired after breakfast" gives you nothing to work with. A detective's entry, on the other hand, tells a story.
Example 1: Vague vs. Detailed
- Vague Entry: "Yogurt for breakfast. Felt foggy."
- Detective Entry: "8:00 AM: 1 cup Greek yogurt with honey and blueberries. 10:30 AM: Mild brain fog (4/10) and feeling sluggish. Lasted about an hour."
Example 2: Connecting Delayed Symptoms
- Vague Entry: "Woke up with a headache."
- Detective Entry: "7:00 AM: Woke up with a dull headache (5/10). Reviewing yesterday's log: 8:00 PM: Large bowl of gluten-free pasta with pesto. Noticed some minor itching before bed."
See how the second example immediately helps connect a morning headache to a meal from the night before? That's a connection that’s almost impossible to make without a detailed log.
Keeping a food journal isn’t about being perfect. It’s about cultivating awareness. You are learning to listen to your body in a structured way, maybe for the very first time.
Tools to Make Tracking Easier
While a simple notebook and pen work just fine, there are plenty of digital tools that can make this process a bit smoother. Many apps are designed specifically for logging food and symptoms, which lets you easily make entries and even spot trends.
Whatever tool you choose, consistency is what will get you results. This focused period of observation is your first real step toward identifying your food sensitivities and will set you up to take targeted action later.
For those who want to narrow down the suspects from the start, the at-home diagnostic panels from BARB N.P. can offer a data-driven starting point, analyzing a wide array of potential food triggers to help focus your detective work.
Mastering the Elimination and Reintroduction Diet
After diligently tracking your food and symptoms, you’ve probably got a shortlist of prime suspects. Now it’s time to confirm those hunches with the gold standard for identifying food sensitivities: the elimination diet.
This isn’t about deprivation. Think of it as a powerful investigation designed to give your body a clean slate. By temporarily removing common culprits, you give your body's inflammatory responses a chance to quiet down. This creates a clear baseline, making it much easier to spot exactly how you feel when a specific food comes back into the picture.
Setting the Stage for the Elimination Phase
The first part of the process is the elimination phase, where you’ll strictly avoid a list of potential trigger foods for a set period. This usually lasts between four and six weeks. The whole point is to remove the foods most commonly linked to sensitivities and see if your symptoms actually improve.
While everyone is unique, a standard elimination diet often starts by removing the "top nine" major allergens. These account for about 90% of all food allergies and a huge number of sensitivities.
- Dairy Products (milk, cheese, yogurt, butter)
- Gluten (wheat, barley, rye)
- Soy (tofu, edamame, soy milk)
- Eggs
- Peanuts and Tree Nuts
- Fish and Shellfish
- Sesame (a recent addition to the major allergen list)
This phase definitely requires careful planning, from prepping your meals to reading every single ingredient label. It can feel like a lot at first, but the clarity you gain is priceless. For a more detailed walkthrough and some practical tips, check out our complete guide to navigating an elimination diet for food allergies.
The Critical Reintroduction Phase
This is where your detective work really pays off—and it’s the step so many people either rush or get wrong. After the elimination period, you’ll start reintroducing the eliminated food groups one at a time. Slowly. Methodically. This systematic approach is the only way to isolate which specific food is causing a reaction.
Here’s a real-world example of how you might reintroduce a single food group, like dairy:
- Day 1: In the morning, have one serving of a pure form of dairy, like a glass of milk or a cup of plain yogurt.
- Days 2-3: Don't eat any more dairy. Go right back to your strict elimination diet and meticulously watch for any symptoms to return—bloating, skin issues, headaches, fatigue, anything.
- Day 4: If no symptoms popped up, you can move on to the next food group (like gluten). If symptoms did appear, you've very likely found a trigger.
It is absolutely vital to track everything in your food diary during this phase. Note the food you ate, the portion size, and any and all symptoms that appear over the next 72 hours.
Rushing the reintroduction phase is like muddying the waters right after you've worked so hard to clear them. Patience here is non-negotiable; it's what provides the definitive answers you're looking for.
Understanding and Managing Skin Reactions
Food sensitivities don't just mess with your gut; they frequently show up on your skin. Issues like acne, rosacea, and eczema can all be fueled by internal inflammation. As you reintroduce foods, pay close attention to any changes in your complexion.
When your gut is inflamed, it can throw your skin's natural balance completely out of whack. Supporting your skin from the outside while you heal from the inside can make a huge difference. The Barb N.P. Facial Mask is an excellent tool for this. It's completely wireless, so it’s comfortable and easy to use while you relax. Its three lighting settings target different concerns: red light helps reduce inflammation, blue light targets acne-causing bacteria, and amber light promotes a healthy glow.
Interpreting the Clues
The data you gather is crucial, especially when you think about how widespread these reactions are. It’s estimated that 6 million children in the U.S. have food allergies—that's about two in every classroom. A significant number of sensitivities often come with a cluster of symptoms, where gut issues occur in 60% of cases and skin problems in 50%. You can discover more insights about food allergy facts and statistics on foodallergy.org.
The simple process of eating, recording what happens, and then analyzing the results is the core of this entire investigation.
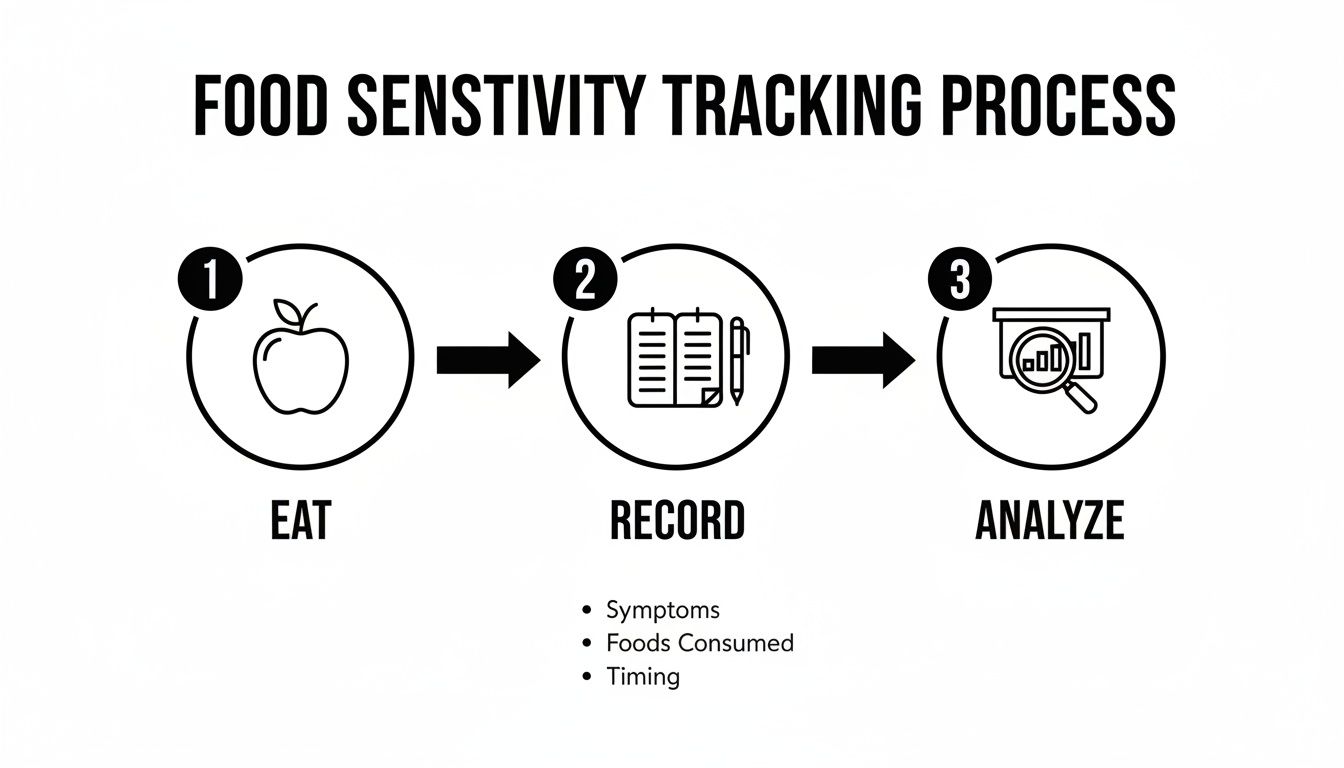
This visual really drives home the simple yet powerful loop of observation and analysis that helps you connect what you eat to how you feel. By following this methodically, you transform guesswork into concrete evidence, empowering you to finally take control of your health.
Using Diagnostic Testing to Guide Your Journey

While a food diary and a classic elimination diet are the gold standard, let's be honest—they demand a ton of patience. It can often feel like you're searching for a needle in a haystack. This is where diagnostic testing comes in, offering a data-driven map to guide your investigation right from the start.
Instead of blindly guessing which foods to pull from your diet, a test can help you build a highly targeted plan. It’s all about working smarter, not harder, by combining your own self-observation with medical-grade insights to get clearer answers, faster.
Demystifying Food Sensitivity Tests
When you start digging into testing options, you’ll find a few different types. The most common at-home tests measure your body’s IgG (Immunoglobulin G) antibody response to a whole host of different foods.
Here's how to think about it: when your immune system is repeatedly exposed to a food it doesn't quite agree with, it can produce IgG antibodies as part of a delayed immune response. An IgG test measures the levels of these antibodies for hundreds of foods, from the usual suspects like dairy and gluten to less obvious things like quinoa or kale.
It’s really important to understand what these tests are—and what they are not.
An IgG food sensitivity test isn't a diagnosis for a true food allergy. Think of it as an incredibly useful tool for flagging potential inflammatory triggers, which then helps you create a much more focused and effective elimination diet.
A high IgG response to a specific food suggests it might be contributing to low-grade inflammation and your symptoms. This insight allows you to prioritize which foods to remove during your elimination phase, potentially shortening the whole discovery process.
The Power of At-Home Testing
The convenience of at-home testing has made this kind of deep insight more accessible than ever before. Brands like BARB N.P. offer comprehensive panels that analyze a huge array of potential food and environmental triggers, all from the comfort of your home.
Here’s how these panels can add real value to your health journey:
- A Data-Driven Starting Point: You get a clear, prioritized list of potential culprits, which takes so much of the initial guesswork out of the equation.
- Targeted Elimination: Instead of cutting out dozens of foods at once, you can focus on the specific items flagged by your test results.
- Faster Insights: By narrowing your focus from the get-go, you can often connect your symptoms to specific triggers more quickly and with greater confidence.
This approach is all about using smart solutions to get to the root of your wellness concerns. You can dive deeper into the nuances and what to look for in a quality test by reading our guide on food sensitivity testing accuracy.
Interpreting Your Results Wisely
It’s crucial to see your test results as clues, not commandments. The number of people dealing with food reactions is huge; the World Health Organization estimates that over 10% of the global population is affected. Yet, a deep dive into 51 different studies showed that while 3-35% of people report having sensitivities, objective tests confirm true rates are closer to 3%.
This gap is exactly why pairing professional testing with your own structured self-observation is the key to getting real, actionable answers.
Beyond just looking at specific foods, understanding your body's general inflammation levels can also provide valuable clues. Getting a clearer picture of your body's overall inflammatory state can help you connect the dots between your diet, symptoms, and overall well-being. This guide on inflammatory markers in blood work is a great resource if you want to learn more.
Ultimately, testing gives you the "what," but a careful reintroduction phase is what confirms the "why." Use your results to build a smarter elimination plan, and then listen to your body’s feedback during reintroduction—that’s always the final verdict.
Building Your Path to Long-Term Wellness and Radiant Skin
Figuring out your food sensitivities is a huge win, but it’s really just the first step. Now comes the part where you turn that knowledge into a sustainable, enjoyable way of life. This isn't about restriction; it's about creating a new foundation for your health—a diet that fuels you without the constant worry of a reaction.
Armed with your list of trigger foods, your relationship with food is about to change. Grocery shopping, dining out, and reading labels will all look a little different. The key is to approach it with a plan, not stress.
Creating Your Sustainable Diet
Lasting change is built on small, smart habits, not a massive overnight overhaul. Focus on simple swaps and mindful planning to make it stick.
- Become a Label Detective: Make reading ingredient lists a non-negotiable habit. Hidden triggers like soy, dairy, and gluten love to hide in unexpected places like sauces, dressings, and even pre-made soups.
- Embrace Whole Foods: Build your meals around things that don't need an ingredient list—fresh fruits, vegetables, lean proteins, and healthy fats. This is the easiest way to sidestep processed additives and hidden triggers.
- Find Your New Favorites: If you find out wheat is an issue, start exploring gluten-free grains like quinoa, rice, and buckwheat. If dairy is out, the world of nut milks and coconut yogurts has exploded with delicious options.
Once you know your triggers, mastering allergy-friendly cooking is your next superpower for making meals that are both safe and genuinely delicious. Resources like guides on mastering allergy-friendly cooking can unlock new recipes and techniques, turning your diet from a list of "can'ts" into a whole new world of culinary possibilities.
The Gut-Skin Connection
Ever notice how a week of digestive upset seems to show up on your face as a breakout? That's not a coincidence. The link between what's happening in your gut and the health of your skin is incredibly direct. Inflammation that starts in your gut from food sensitivities can manifest as visible skin problems.
When your body reacts to a trigger food, it can set off an inflammatory chain reaction that echoes throughout your entire system. That’s why calming your gut is one of the most powerful things you can do for your complexion.
Many people I've worked with are shocked to see chronic skin issues like acne, rosacea, and eczema start to clear up once they remove their trigger foods. A calmer gut almost always leads to clearer, more radiant skin.
This internal healing is powerful, but you can absolutely support your skin's recovery from the outside, too. Pairing your dietary changes with targeted skincare can amplify your results, helping to soothe inflammation and bring your skin back into balance.
Enhancing Your Skin's Radiance
As your internal system quiets down, you can give your skin an extra boost to help it heal and get its glow back. This is where a targeted, at-home treatment can make a world of difference, addressing the lingering effects of inflammation right at the source.
We recommend the Barb N.P. LED Facial Mask as the perfect partner to your new wellness-focused lifestyle. It’s an effortless way to support your skin’s recovery at home, helping to dial down the visible signs of inflammation and promote a clearer complexion.
What makes it so effective is its thoughtful, practical design:
- Total Convenience: The mask is completely wireless, so you can move around, read, or just relax during your treatment without being tethered to a wall.
- Unmatched Comfort: It’s designed to fit the contours of your face comfortably, making it an easy and pleasant ritual to stick with.
- Targeted Treatments: With three distinct lighting settings, you can customize your session. Red light is fantastic for calming inflammation, blue light helps target acne-causing bacteria, and amber light works to rejuvenate the skin for a healthy glow.
Using a tool like this alongside your new diet creates a powerful two-pronged attack. You’re healing your body from the inside out while supporting your skin from the outside in—paving the way for lasting wellness and that truly radiant complexion you're after.
Common Questions About Food Sensitivities
As you dive into the world of food sensitivities, it's completely normal for questions to bubble up. This whole process can feel a little overwhelming at first, but getting clear answers is the key to feeling confident and in control of your health.
Let's walk through some of the most common questions I hear from people just starting this journey.
How Long Does It Really Take to See a Difference?
This is probably the number one question people have. While you might start feeling some initial relief within the first week of an elimination diet, the real magic happens over time.
It typically takes at least three to four weeks for your body's inflammatory response to fully calm down. This is crucial because it allows you to establish a true, clean baseline before you even think about reintroducing foods one by one. Patience here is everything.
Can I Suddenly Develop a New Food Sensitivity?
Absolutely. In fact, it's incredibly common for adults to develop sensitivities to foods they've eaten their entire lives without a single issue. This isn't like the childhood allergies you often hear about; adult-onset sensitivities are a different beast altogether.
What causes this shift? It can be anything from a change in your gut health, a period of chronic stress, hormonal fluctuations, or even just a round of antibiotics that threw your system off balance. A food that was once a daily staple might suddenly become the source of your bloating, headaches, or skin flare-ups. Your body is always adapting, and its responses can change right along with it.
Your body is constantly communicating with you. The real goal here isn't just to find a "problem" food, but to learn how to listen more closely to what your body needs at every stage of your life.
This is why staying aware is so important. A food that’s perfectly fine for you today might become a trigger five years from now—and sometimes, a past trigger can even become tolerable again.
What’s the Difference Between a Test and a Diagnosis?
This is a critical distinction that trips a lot of people up. An at-home food sensitivity panel is a tool, not a final diagnosis in the way a true food allergy test is.
Let’s break it down:
- A Food Sensitivity Test: This kind of test, which measures your IgG antibody levels, is designed to spot potential inflammatory responses to certain foods. Think of it as a data-gathering tool. It gives you a prioritized list of suspects to investigate further through a structured elimination diet.
- A Food Allergy Test: This is performed by an allergist (think skin prick tests or IgE blood tests) and confirms an immediate, IgE-mediated immune reaction. This is the kind of severe response that causes hives, swelling, or even life-threatening anaphylaxis.
An at-home sensitivity panel is your roadmap for the detective work ahead. It provides the clues you need to form a solid hypothesis. The actual "diagnosis"—or confirmation—of a sensitivity comes from your direct experience during the elimination and reintroduction phases, where you connect a specific food to your specific symptoms.
This is where at-home panels become so valuable. Instead of randomly guessing which foods to cut out, a test from BARB N.P. helps you create a targeted, efficient elimination plan right from the start. It saves you a ton of time and frustration on your path to feeling better.
At BARB N.P., our goal is to give you the tools and insights to take back control of your wellness. Our at-home diagnostic tests are designed to provide a clear, data-driven starting point for understanding your body's unique needs. Explore our testing options today and begin your journey to a healthier you.

