
When you're trying to pinpoint the cause of your allergies, the choice between a blood test vs. a skin test often comes down to your personal health, lifestyle, and even the medications you're taking.
An allergy blood test, for instance, measures specific IgE antibodies in your bloodstream from a single sample. This makes it a perfect fit if you have a skin condition like eczema that would interfere with a skin test, or if you simply can't stop taking medications like antihistamines.
On the other hand, a skin test gives you answers much faster, but it requires pricking your skin with tiny amounts of allergens and means you'll have to pause those antihistamines for several days beforehand.
Comparing The Two Main Types of Allergy Tests
Navigating allergy diagnostics means choosing between two primary methods. Each test is designed to identify the specific triggers behind your reactions, but they get there in completely different ways. Understanding these differences is the first step toward making a smart, informed decision with your healthcare provider.
The right choice often hinges on your unique circumstances. Things like your current health status, any medications you're taking, the condition of your skin, and even your age can make one test a much better option than the other.
Quick Comparison: Allergy Blood Test vs. Skin Test
To make things simple, let's break down the practical differences you can expect from each test. This table gives you a clear, at-a-glance look at what sets them apart.
| Feature | Allergy Blood Test (Specific IgE) | Allergy Skin Test (Prick Test) |
|---|---|---|
| Method | A single blood sample is drawn and sent to a lab for analysis. | Small amounts of allergens are pricked into the skin's surface. |
| Medication Interference | Minimal; you can continue taking most medications, including antihistamines. | Requires stopping antihistamines 3-7 days before the test. |
| Patient Suitability | Ideal for infants, patients with severe eczema, or those on interfering meds. | Not suitable for those with widespread skin conditions or dermatographism. |
| Result Speed | Results typically take several days to a week. | Immediate results are visible in about 15-20 minutes. |
| Safety Risk | Virtually no risk of an allergic reaction during the test. | Small but present risk of a systemic allergic reaction. |
This quick rundown highlights the key trade-offs: blood tests offer convenience and safety for certain individuals, while skin tests provide rapid, real-time results.
This infographic helps visualize the decision-making process, especially when factors like medication use and skin health are a concern.
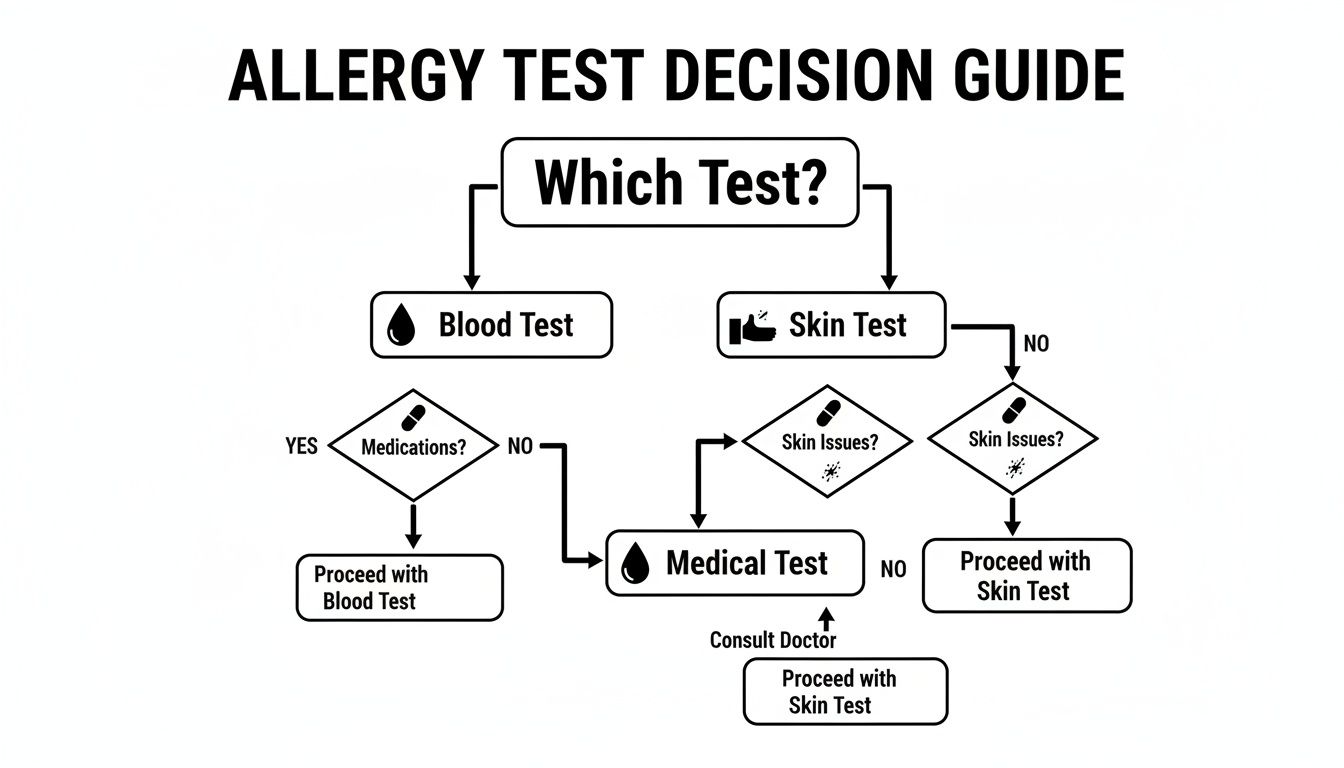
As you can see, if you have a skin condition or can't stop taking antihistamines, a blood test is clearly the recommended path forward.
Making an Informed Choice with Barb N.P.
While the table gives a great overview, the best test for you really depends on a detailed look at your health history and lifestyle. The growing convenience of at-home allergy testing, like the comprehensive panels offered by Barb N.P., makes the blood test an increasingly popular and practical choice. These panels let you gather critical health data right from the comfort of your home.
Ultimately, discussing these factors with an expert like Barb N.P. ensures your testing strategy is perfectly aligned with your needs. The goal is simple: get accurate, actionable information with the greatest safety and convenience to build an effective treatment plan.
How Each Allergy Test Works: Skin vs. Blood
To figure out whether a blood test or skin test is right for you, you first need to understand how they work. While both are designed to pinpoint your allergic triggers, they get there in completely different ways. One is a direct, real-time challenge to your skin, while the other is more of an investigation into your immune system's memory.
Think of it like this: a skin test is like asking your body, "Are you allergic to this?" and getting an immediate, visible answer. A blood test is more like detective work, analyzing your blood for the immunological "fingerprints" left behind from past encounters with allergens.
The Skin Prick Test: A Direct Approach
The skin prick test (SPT) is the classic allergy test you've probably seen before, and it’s always done in a clinic. It’s a direct method that measures an immediate allergic reaction, known as a Type I hypersensitivity.
The process is pretty straightforward:
- Prep: A nurse or doctor cleans a patch of skin, usually on your forearm or back.
- Application: They place tiny droplets of purified liquid allergens on your skin—things like pollen, mold, pet dander, or specific foods.
- Introduction: Using a small, sterile plastic device, the provider gently pricks or scratches the skin's surface through each droplet. This lets a minuscule amount of the allergen seep just below the skin.
If you’re allergic, your immune system flags that substance as a threat. Mast cells in your skin immediately release histamine and other chemicals, causing a small, raised, red bump called a wheal to pop up within 15-20 minutes. The size of that wheal is then measured to figure out your level of sensitivity.
The Specific IgE Blood Test: An Indirect Investigation
An allergy blood test, often called a specific IgE (sIgE) test, works indirectly. Instead of putting allergens on your skin, it measures the amount of specific Immunoglobulin E (IgE) antibodies floating in your bloodstream.
The process involves a single blood draw, which is then sent off to a lab. There, your blood serum is mixed with various suspected allergens. If your blood contains IgE antibodies specific to something like peanuts or ragweed, those antibodies will bind to the allergen, signaling a positive result.
The biggest advantage of a blood test is that it's quantitative. It doesn't just give a "yes" or "no"—it provides a precise measurement of IgE antibodies, which helps your doctor gauge just how sensitized you are.
Modern lab methods, like the ImmunoCAP test, are incredibly sensitive and can detect even tiny levels of these antibodies. This gives you objective, measurable data that can be tracked over time to see if your allergies are changing.
What This Means for You as a Patient
When you're deciding between the two, your comfort and current health status are key. A skin prick test involves multiple small pricks, which can be annoying for young kids or anyone who isn't a fan of needles. It can also get pretty itchy.
A blood test, on the other hand, is just a single needle poke. For anyone dealing with chronic skin issues like eczema, hives, or psoriasis, avoiding any extra skin irritation makes the blood test a much smarter choice. This is also why many aesthetic professionals, like Barb N.P., might suggest it before certain skin treatments to prevent a flare-up.
When your skin's health is the priority, you need tools that calm and support its natural barrier. The Barb N.P. LED Facial Mask is perfect for this. Its comfortable, wireless design makes it easy to manage skin reactivity at home. The mask features three different light settings—including anti-inflammatory red and blue light—to soothe irritation, prepping your skin for aesthetic procedures or just keeping it healthy, especially if you’re prone to allergic skin reactions.
Analyzing Accuracy And Reliability In Allergy Testing
When it comes to choosing between an allergy blood test and a skin test, the first question everyone asks is: "Which one is more accurate?" A reliable diagnosis is, after all, the cornerstone of an effective treatment plan. Both methods are valuable tools, but they work differently, measuring separate parts of your immune response.
Skin tests are all about the immediate, visible reaction. By introducing a tiny amount of an allergen to the skin, we can watch for a localized response—the classic wheal-and-flare bump. It's direct, but the interpretation is visual and can be subjective.
Blood tests, on the other hand, give us objective, hard data. They measure the exact amount of specific IgE antibodies circulating in your bloodstream, providing a quantitative value that we can track over time. This offers a more analytical look at your body's sensitization levels.
Sensitivity and Specificity Explained
To really dig into accuracy, we have to talk about two key metrics: sensitivity and specificity.
- Sensitivity is a test’s ability to correctly identify someone who actually has an allergy. Think of it as its power to find a true positive. A highly sensitive test rarely misses a real allergy.
- Specificity is a test's ability to correctly rule out an allergy in someone who doesn't have one. This is its power to find a true negative. A highly specific test rarely gives a false positive.
For years, skin prick tests were seen as the gold standard, often praised for their high sensitivity. But technology doesn't stand still. Modern blood tests have made huge strides in the last two decades. Today’s advanced tests show impressive sensitivity rates from 70% to 90% and specificity rates ranging from 40% to 100%. These are no longer just screening tools; they are precise diagnostic instruments.
The Importance of Clinical Context
Here's the most critical piece of the puzzle: a positive result from either a blood or skin test doesn't automatically mean you have a clinical allergy. What it confirms is sensitization—your immune system has created IgE antibodies against that substance. You can be sensitized to something without ever having an allergic reaction to it.
Key Takeaway: Both blood and skin tests detect sensitization, not a guaranteed allergy. This is why a professional interpretation that combines your results with your medical history and symptoms is non-negotiable for a correct diagnosis.
For example, your test might come back positive for a specific grass pollen, but you only ever feel symptoms during its peak season. Conversely, a positive test for a food you eat all the time without any issues is probably just sensitization, not a true allergy that requires you to avoid it. For a deeper look into this, check out our guide on how accurate allergy tests are.
Factors That Can Influence Your Test Results
The reliability of any allergy test isn't just about the test itself; several factors can sway the results.
- The Allergen Itself: Testing for inhaled allergens like pollen, mold, and dust mites tends to be very reliable with both methods. Food allergy testing, however, can be far more complex, sometimes yielding less straightforward results.
- Patient-Specific Factors: Your age, existing skin conditions like eczema or psoriasis, and even the location on your body used for a skin test can affect the outcome. Blood tests neatly sidestep these issues, making them a more consistent choice for anyone with chronic skin problems.
- Medication Interference: This is a big one. Antihistamines work by blocking the allergic response, which means they will almost certainly cause a false negative on a skin test. This is a major reason why blood tests are the go-to for patients who can't safely stop their daily allergy medications.
Ultimately, the most accurate diagnostic path is one guided by a skilled professional, like Barb N.P., who can choose the right test for your unique situation and interpret the results within the full context of your health and lifestyle.
The Patient Experience: Safety And Preparation
When it comes to choosing between an allergy blood test and a skin test, the practical side of things often makes the decision for you. It’s not just about the science; it’s about your comfort, safety, and what fits into your life. One path is straightforward, while the other requires you to plan ahead and even pause your daily medications.
A skin prick test demands that you actively prep your body. The biggest step is stopping all antihistamines for 3 to 7 days beforehand. These medications are designed to block the very reactions the test is trying to trigger, so taking them would completely skew the results and lead to false negatives.
For anyone who relies on daily allergy medication to get through the day, this can be a deal-breaker.

Safety Profiles: Skin Test vs. Blood Test
The two tests have completely different safety considerations. A skin test, by its very nature, involves introducing tiny amounts of potential allergens into your body, which always carries a small but real risk.
- During the Test: You can expect some temporary itching, redness, and raised bumps where you react. That’s actually a sign it’s working, but for some, the discomfort can be significant.
- Systemic Reaction Risk: Although it's rare, there's a slight chance of a more severe, body-wide allergic reaction called anaphylaxis. This is exactly why skin tests must be done in a medical office where a team is ready to respond immediately.
A blood test, on the other hand, is an ex vivo procedure—meaning it all happens in a lab tube, completely separate from your body. The single blood draw carries zero risk of causing an allergic reaction. This inherent safety makes it the go-to choice for anyone with a history of severe allergies or for testing high-risk triggers.
The core safety difference is simple: a blood test analyzes your immune system's potential without exposing you to any risk, whereas a skin test creates a controlled exposure to gauge a live reaction.
Convenience And Comfort
Beyond the safety aspect, convenience plays a huge role. For many people, the allergy blood test is just plain easier. You don't have to stop taking antihistamines or most other medications. You can just carry on with your normal routine without any disruption.
This is a massive advantage for people with chronic conditions or those who simply can't go a week without their allergy meds.
For patients with widespread skin conditions like severe eczema or dermatographism—a condition where skin welts easily from minor scratches—a blood test isn't just more convenient, it's often the only real option. Performing a skin test on already reactive skin would make the results impossible to read accurately. Properly equipping a facility for these procedures is crucial; for more on finding the right lab equipment for medical testing, there are specialized resources available.
When your skin is reactive, proactive care at home is just as important. The Barb N.P. LED Facial Mask is an excellent tool for calming inflammation and supporting overall skin health, especially for those prone to allergic skin issues. Its comfortable, wireless design and three light settings—including an anti-inflammatory red light—offer a soothing, professional-grade treatment. It’s a fantastic way to complement an allergy management routine by keeping your skin calm and resilient.
Evaluating Cost, Access, And Real-World Scenarios
When you’re weighing an allergy blood test vs skin test, the conversation goes far beyond just accuracy. Practical things like cost, insurance coverage, and real-world convenience often become the deciding factors. While skin tests have long been the in-office standard, a closer look at the bigger picture reveals that a blood test is often the smarter, more efficient choice.
Think about it: one blood test can deliver a whole panel of results without chaining you to multiple specialist appointments. That convenience alone can add up to serious savings in time and money. When you factor in taking time off work, co-pays, and follow-up visits for skin testing, the initial sticker price doesn't tell the full story.
Comparing Financial Outlays And Insurance
At first glance, a skin prick test might seem cheaper than a lab-analyzed blood test. But insurance coverage is the great equalizer. Most plans cover both types of allergy testing, though the specifics can vary, so it’s always smart to check with your provider first to understand what you’ll pay out-of-pocket.
The real financial story unfolds over time. A comprehensive study on healthcare utilization revealed that blood allergy testing is tied to significantly lower long-term costs, mainly because it cuts down on the need for specialist visits. Patients who only had a serum IgE test averaged just 0.6 allergist visits in the following year. In contrast, those who only had skin testing averaged 4.2 visits.
That’s a difference of 3.2 fewer specialist appointments, a massive reduction in the overall healthcare burden.
While a skin test might look like the budget option upfront, the blood test often proves more cost-effective and convenient in the long run by minimizing repeat consultations and follow-ups.
When To Choose A Blood Test
Some situations just aren't a good fit for skin testing. These aren't rare exceptions—they are common scenarios where a blood test is the clear winner for safety, accuracy, and practicality.
- Infants and Young Children: A single, quick blood draw is far less traumatic and much easier to manage for little ones than the series of scratches a skin test requires.
- Patients with Severe Skin Conditions: If you’re dealing with widespread eczema, psoriasis, or dermatographism, your skin is already reactive. A skin test would be unreliable at best and could easily make your condition worse.
- Individuals Unable to Stop Antihistamines: Many people depend on daily antihistamines to function. Asking them to stop for a week simply isn't an option. A blood test lets them continue their medication without a problem.
- History of Severe Allergic Reactions: For anyone with a history of anaphylaxis, a blood test is the only safe choice. It carries zero risk of triggering a dangerous systemic reaction during the test itself.
For those looking for a modern and reliable diagnostic solution, learning more about how to allergy test at home can be a game-changer.
When A Skin Test Might Be Preferred
Despite the clear benefits of blood testing, the skin test still has its place, and its main advantage is speed. In an allergist's office, you can get results from a skin test in just 15-20 minutes. That immediate feedback allows the doctor to discuss a treatment plan with you in the very same visit.
This is great for straightforward cases where the patient has no other complicating factors. However, for a growing number of people, the combination of safety, convenience, and comprehensive results makes an allergy blood test the more practical and forward-thinking path.
How Allergy Testing Elevates Your Aesthetic Treatments
You might be surprised to learn how closely your allergies are tied to the success of your aesthetic treatments. When your body is dealing with chronic, low-grade inflammation from hidden allergies—whether to food, skincare, or pollen—it creates a tricky foundation for procedures like fillers, lasers, and microneedling. This constant immune response can show up as eczema, hives, or stubborn redness, making treatments more complicated and undermining your results.
Pinpointing these secret triggers is one of the smartest things you can do to ensure both safety and stunning outcomes. When your immune system is calm, your skin heals faster, responds better to treatments, and holds onto that radiant glow much longer. This is exactly where the allergy blood test vs skin test conversation becomes so important for anyone invested in their aesthetic wellness.

Why At-Home Blood Tests Are a Game-Changer Before Procedures
For anyone planning an aesthetic treatment, an allergy blood test has some serious perks. It gives you a complete overview of potential sensitivities without making existing skin issues worse. This is a big deal, since a traditional skin prick test could easily cause an eczema or hive flare-up, pushing your treatment schedule back even further.
This is why at-home testing, like the panels offered by Barb N.P., is such a powerful first step. You can gather critical information about your body’s sensitivities from the comfort of your home, giving you a clear map of potential triggers before you even set foot in a clinic. Knowing your allergens helps you make smarter choices about your skincare and diet, building a stronger, more stable canvas for any aesthetic work.
Taming Allergic Skin for a Better Glow
Once you know what your triggers are, managing your skin's reactivity gets a whole lot easier. A holistic game plan that combines avoiding allergens with supportive skincare tech is where the magic happens. The goal is simple: calm the inflammation to prep your skin for treatments and keep it healthy long after.
For at-home care, the Barb N.P. LED Facial Mask is an incredible tool. It’s completely wireless, so you can move around freely during your session, and it’s designed for supreme comfort.
The mask’s three light settings, including anti-inflammatory red and calming blue light, are engineered to soothe irritation, dial down redness, and support your skin’s healing process. It's the perfect ally for allergy-prone skin.
Using this mask regularly helps build up your skin’s resilience, making it less likely to have flare-ups that could get in the way of your aesthetic goals.
Historical research comparing skin prick tests to serum IgE blood tests confirms that while both are reliable, they each have unique strengths. For example, one major study of 794 patients found that dust mites (Dermatophagoides pteronycinus) were the most common culprit, identified in 54.4% of patients with a skin prick test. This shows that while both tests are valuable, the right choice depends on your specific situation, and a skilled practitioner will always correlate the results with your personal history to get the full picture. You can learn more about these comparative findings and what they mean for patients.
Ultimately, weaving allergy awareness into your aesthetic plan is a brilliant strategy. By proactively identifying and managing your triggers with tools like the Barb N.P. at-home test and supporting your skin with calming tech like the LED Facial Mask, you’re creating the absolute best conditions for achieving gorgeous, lasting results.
Your Top Questions About Allergy Testing Answered
When you're trying to get to the bottom of your symptoms, it's natural to have questions. Let's clear up some of the most common ones about the allergy blood test vs skin test so you can feel confident in your diagnostic journey.
Can An Allergy Blood Test Be Wrong?
Yes, it's possible—no medical test is 100% foolproof. An allergy blood test can sometimes show a false positive, meaning you have IgE antibodies to a substance but don't actually react to it in real life. It can also produce a false negative.
This is why we say a positive test confirms sensitization, not necessarily a clinical allergy. The real diagnosis comes when a professional puts those results in context with your specific symptoms and medical history. For a deeper dive, check out our guide on how to make sense of your results: interpreting allergy test results.
Which Test Is Better For Food Allergies?
While both methods work, blood tests are often the smarter choice for food allergies for a few key reasons. First and foremost, they're safer because there's zero risk of triggering a severe allergic reaction, which is a real concern with skin testing for potent food allergens.
They're also far more practical for little ones or for anyone with widespread eczema, a condition that can make skin prick tests unreliable.
How Long Do Allergy Test Results Take?
This is where the two tests really differ. With a skin test, you get your answers on the spot. The results develop right there on your skin in about 15-20 minutes.
A blood test, on the other hand, needs to be sent off to a lab for analysis. You can usually expect to hear back with your results in a few days to a week.
Once you have your results, creating an allergen-free home is a great next step. Many people find relief by investing in tools like the best air purifiers for allergies to improve their indoor environment.
Here at BotoxBarb, we know that true radiance starts from within. Managing inflammation is a cornerstone of achieving healthy, beautiful skin. That's why we love the Barb N.P. LED Facial Mask, an at-home device designed to soothe and support your complexion. Its wireless design and three therapeutic light settings help calm reactivity, making it a perfect addition to your routine if you have sensitive or allergy-prone skin.
Explore our curated wellness solutions at https://barbnp.shop.

